Understanding Osteoporotic Vertebral Compression Fractures: Causes, Symptoms, and Treatment Options
As we age, our bones naturally lose strength and density. For many adults—especially women over 60—this process can lead to osteoporosis, a condition where bones become fragile and more prone to fractures. One of the most common and painful consequences of osteoporosis is a vertebral compression fracture (VCF), which affects the bones in the spine.
What Is a Vertebral Compression Fracture?
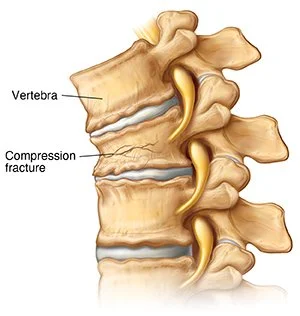
A vertebral compression fracture occurs when one of the vertebral bodies—the building blocks of your spine—collapses or compresses under pressure. In patients with osteoporosis, even minimal trauma or everyday activities like bending, lifting a light object, or sneezing can result in a fracture.
These fractures are most common in the mid-to-lower back (thoracic and lumbar spine) and often go undiagnosed or mistaken for routine back pain.
Symptoms
Sudden onset of back pain, often sharp or burning
Worsening pain when standing or walking, improved with lying down
Height loss or a stooped posture (“dowager’s hump”)
Pain localized to one area of the spine
Limited mobility or difficulty with daily activities
In some cases, patients don’t realize they’ve fractured a vertebra and assume the pain is due to muscle strain or arthritis.
Who Is at Risk?
Postmenopausal women with osteoporosis
Men over age 65 with low bone density
Individuals on long-term steroid medications
Patients with a history of cancer or prior spine fractures
Those with low body weight or poor nutrition
If you’ve been diagnosed with osteoporosis, your risk of spine fracture increases significantly with age. One vertebral fracture also increases the chance of a second fracture in the future.
How Is It Diagnosed?
Diagnosis typically involves a combination of:
Physical exam
Spinal X-rays to visualize collapse or compression
MRI to assess for edema (acute vs. chronic fracture) and rule out malignancy
DEXA scan to evaluate bone density and confirm osteoporosis
Treatment Options
Most compression fractures heal without surgery, but proper diagnosis and a tailored treatment plan are essential.
Conservative Management:
Activity modification (avoid bending/lifting)
Medications: pain relievers, anti-inflammatory drugs
Osteoporosis treatment (bisphosphonates, calcium, vitamin D)
Physical therapy once pain improves
Minimally Invasive Surgery:
If pain persists or the fracture leads to significant spinal deformity or loss of mobility, surgical options may be appropriate:
Kyphoplasty – Similar to vertebroplasty, but includes inflation of a balloon to restore vertebral height before cement placement.
These outpatient procedures are typically quick, low-risk, and can offer rapid pain relief.
Long-Term Outlook
With early diagnosis and proper treatment, most patients experience significant pain relief and return to normal activities. Preventing future fractures through bone health optimization—including nutrition, exercise, and osteoporosis treatment—is critical.
If you or a loved one is experiencing persistent back pain, especially after a minor injury or if you’ve been diagnosed with osteoporosis, don’t ignore it. A simple evaluation can determine whether a vertebral compression fracture is present—and whether treatment can relieve pain and prevent further damage.